Systemic vs. Localized Inflammation: Understanding the Differences
Inflammation is a term used in common nomenclature but can have different meanings. Understanding systemic and localized inflammation is a good place to start.
Inflammation is a natural defense mechanism the body uses to protect itself from harm, such as infections, physical injury, or chemical injury. It is a healing process. If it persists or occurs uncontrolled, it may actually become harmful. Localized inflammation occurs at an injury or infection site, whereas systemic inflammation affects the entire body.
What is Inflammation?
Inflammation is a complex biological response involving the immune system, blood vessels, and molecular mediators like cytokines and chemokines. Various stimuli, including pathogens, damaged cells, and toxic chemicals can trigger it. The goal of inflammation is to eliminate the initial cause of cell injury, clear out damaged cells and tissues, and repair the damaged cells or tissues.
Cytokines and chemokines are proteins that act like messengers in the immune system. In a simplified description, cytokines regulate immune cell activity, while chemokines attract immune cells to where they are needed.
The five signs of inflammation are redness, heat, swelling, pain, and loss of function. These symptoms are commonly associated with localized inflammation, but they can be less evident in systemic inflammation.
Localized Inflammation: A Targeted Response
Localized inflammation occurs at the site of injury or infection. When tissues are damaged, immune cells, such as neutrophils and macrophages, are rapidly recruited to the area. Inflammatory mediators increase blood flow (dilating blood vessels), vascular permeability (so more plasma leaks out of the blood vessels into the extracellular space), and the migration of white blood cells into the tissue (Libby, 2007). This local response is essential to isolate the injury or infection, destroy pathogens, and initiate tissue repair.
Increased blood flow: causes redness and heat
Vascular permeability: causes swelling, resulting in pain and loss of function (Libby, 2007)
Note that localized inflammation is a healing process. Anti-inflammatory treatments, such as cold (ice packs) and NSAIDs (ibuprofen or naproxen) can relieve pain, but may negatively affect healing.
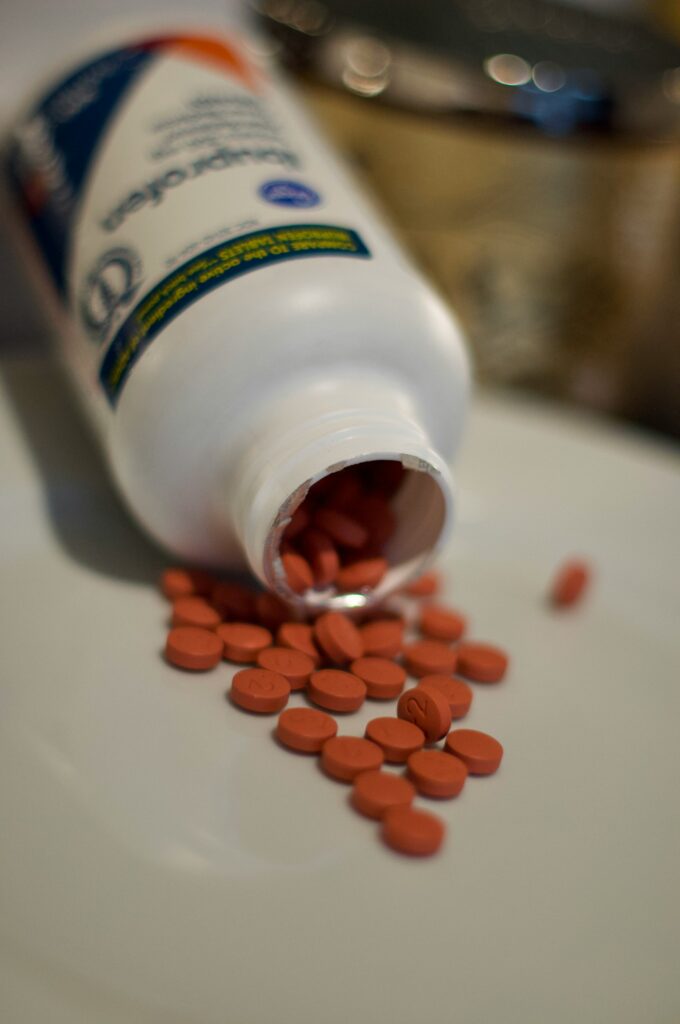
Exercise can result in temporary muscle soreness, a localized inflammatory response. Treating with anti-inflammatory medications (NSAIDs) may reduce healing and improve the strength and endurance sought from physical training (Lundberg & Howatson, 2018).
Systemic Inflammation: A Widespread Response
Systemic inflammation, on the other hand, involves a broader immune response. Instead of being confined to one specific area, systemic inflammation can affect multiple organs and systems, leading to widespread effects. It can be triggered by severe infections, autoimmune diseases, chronic stress, obesity, and certain lifestyle factors (Hotamisligil, 2006; Galland, 2000).
Characteristics of Systemic Inflammation
- Body-wide involvement: Unlike localized inflammation, systemic inflammation affects the entire body. The inflammatory mediators released into the bloodstream travel to multiple organs, potentially causing widespread damage.
- Chronic nature: Systemic inflammation is often chronic and low-grade, persisting over a long period without overt symptoms. Chronic systemic inflammation is associated with many diseases, including cardiovascular disease, diabetes, cancer, and autoimmune conditions.
- Subtle signs and symptoms: While acute systemic inflammation, such as sepsis (infection in the blood), can produce apparent and life-threatening symptoms (fever, rapid heart rate, organ dysfunction), chronic systemic inflammation is more insidious. It may not produce overt signs of illness. Subtle signs and symptoms such as fatigue, weight gain, cognitive decline, or increased susceptibility to infections can be challenging, even for clinicians, because the cause is often not apparent.
- Mediated by cytokines: Systemic inflammation is heavily driven by the release of pro-inflammatory cytokines, including tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and C-reactive protein (CRP) (Hotamisligil, 2006). Elevated levels of these markers in the blood are commonly used as indicators of systemic inflammation. However, these markers of inflammation are “non-specific,” not pointing to a clear diagnosis or cause.
- Common causes: Systemic inflammation can be triggered by a wide variety of factors, including chronic infections (e.g., HIV, hepatitis), autoimmune diseases (e.g., lupus, multiple sclerosis), metabolic syndrome (e.g., obesity, type 2 diabetes), exposure to environmental toxins, and dietary choices.
Differences in Inflammatory Pathways
- Localized inflammation: In localized inflammation, cytokines primarily act at the injury site, which induces vascular changes and recruits immune cells. The local environment can contain the inflammatory response.
- Systemic inflammation: In systemic inflammation, cytokines are released into the bloodstream, traveling throughout the body and affecting distant organs. Excess oxidative stress may be a contributing factor to the initiation of systemic inflammation (Theodosis-Nobelos & Rekka, 2024). The widespread nature of systemic inflammation can lead to more profound damage and chronic disease states.
The Role of Chronic Inflammation in Disease
Chronic systemic inflammation is now recognized as a major factor in the development and progression of many chronic diseases. Unlike acute localized inflammation, which is protective and healing, chronic systemic inflammation can lead to tissue damage, organ dysfunction, and the promotion of conditions such as cardiovascular disease, diabetes, cancer, and others (Medzhitow, 2008). The increasing prevalence of these diseases is related to the immune system’s response to obesity from excess adipose tissue (body fat). Adipose tissue can build with excess caloric intake and lack of exercise. A diet high in fat likely increases oxidative stress to tissues resulting in an inflammatory response (Theodosis-Nobelos & Rekka, 2024). Adipose tissue also creates an environment of oxidative stress, promoting systemic inflammation.
Conclusion
Localized inflammation is a short-term, protective response confined to a specific body area and part of the healing process. Systemic inflammation is a more generalized response that can affect the entire body, can be progressive, and potentially harmful. Systemic inflammation, especially when chronic, plays a significant role in the development of many diseases. Systemic inflammation can also cause non-specific symptoms that make an otherwise healthy person feel ill.
References:
- Galland L. (2010). Diet and inflammation. Nutrition in clinical practice: official publication of the American Society for Parenteral and Enteral Nutrition, 25(6), 634–640.
- Hotamisligil G. S. (2006). Inflammation and metabolic disorders. Nature, 444(7121), 860–867.
- Libby P. (2007). Inflammatory mechanisms: the molecular basis of inflammation and disease. Nutrition reviews, 65(12 Pt 2), S140–S146.
- Lundberg, T. R., & Howatson, G. (2018). Analgesic and anti-inflammatory drugs in sports: Implications for exercise performance and training adaptations. Scandinavian journal of medicine & science in sports, 28(11), 2252–2262.
- Medzhitov R. (2008). Origin and physiological roles of inflammation. Nature, 454(7203), 428–435.
- Theodosis-Nobelos, P., & Rekka, E. A. (2024). The Antioxidant Potential of Vitamins and Their Implication in Metabolic Abnormalities. Nutrients, 16(16), 2740.
Photos:
- Featured Photo by National Cancer Institute on Unsplash
- Ibuprofen Photo by Dan Dennis on Unsplash

Join Our Mailing List
Good timing on this! I will reconsider my choice on taking NSAIDs after the marathon I ran today 👏 😉 … and let my body heal. Thanks for the article MedFitConsulting!
Thanks for reading, and the comment!